TMJ refers to Temporomandibular joint and muscle disorders, also known as TMJ dysfunction or TMJ disorder, which are grouped conditions that together lead to lack of proper function and pain in the joint of your jaw and the muscles that control its movement. The exact cause of TMJ disorders is often unknown and can be complex, involving multiple factors. These disorders can affect the facial muscles and chewing muscles, both of which play a role in TMJ symptoms. The muscles that control jaw movement are essential for proper jaw function, and dysfunction in these muscles or the joint can lead to significant discomfort. According to some estimates, TMJ affects over 10 million Americans. The TMJ structure is complex, and variations in its structure can influence the development and severity of TMJ disorders. If you have jaw pain or symptoms of TMJ, consult an oral professional for the most accurate diagnosis as most jaw pain does not signify TMJ and is temporary or needs only minor treatment.
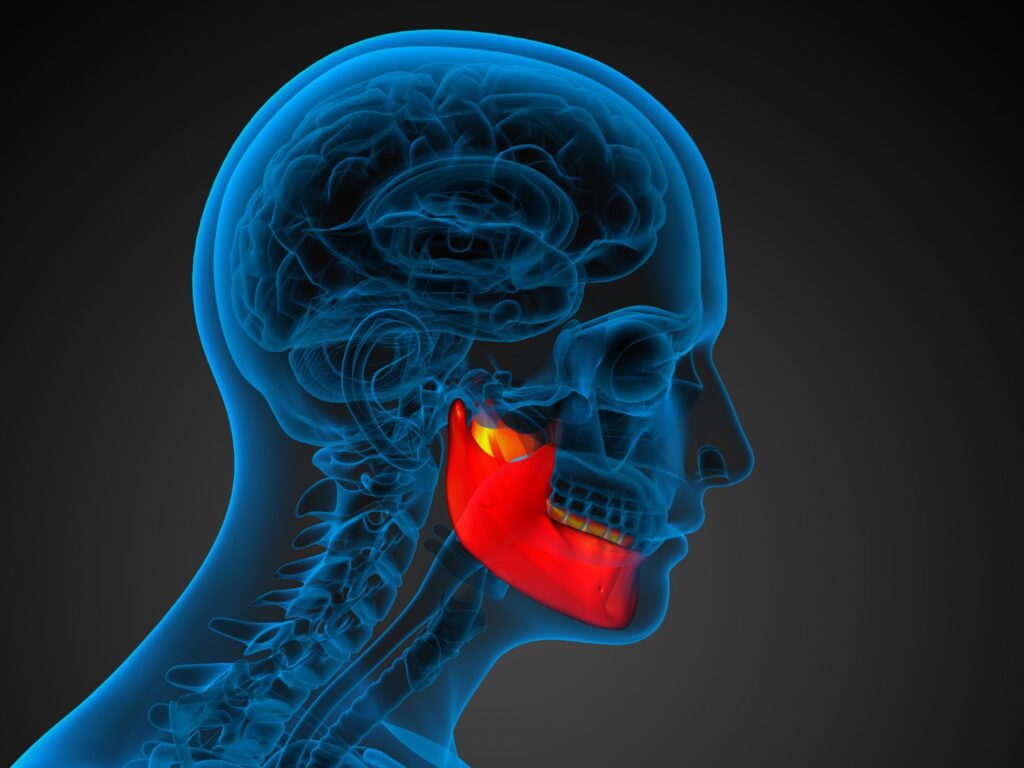
What is the Temporomandibular Joint (TMJ)?
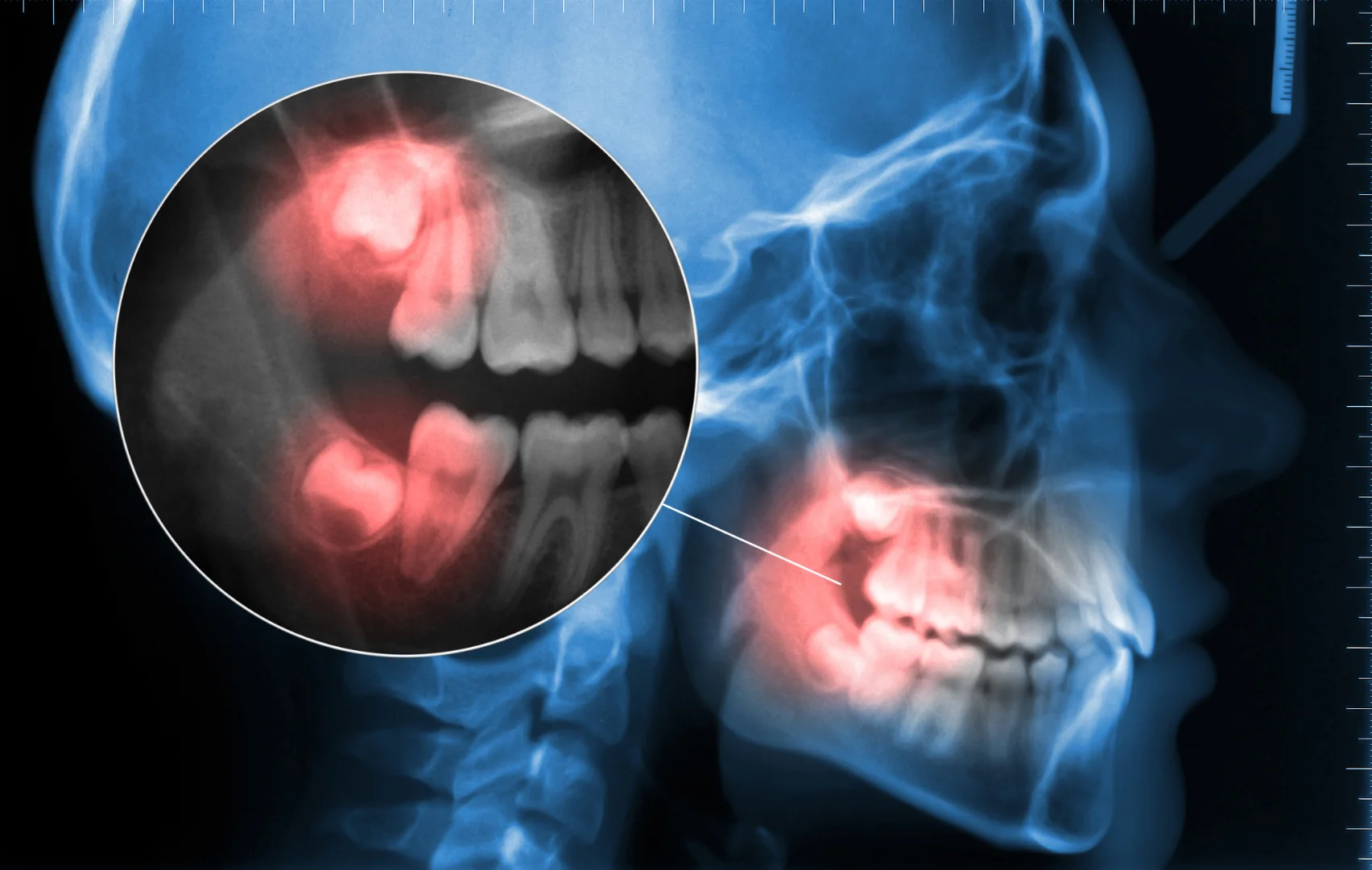
The temporomandibular joint (TMJ) is a unique and complex hinge that connects your lower jaw, or mandible, to the temporal bones on each side of your skull. Located just in front of your ears, the temporomandibular joint TMJ allows for the smooth movement of your jaw, making it possible to talk, chew, yawn, and perform other essential functions. Because the TMJ is involved in nearly every jaw movement throughout the day, it is one of the most frequently used joints in the body. This constant use makes the TMJ susceptible to wear, injury, and various disorders that can lead to discomfort or pain. Understanding how this joint works is key to recognizing and addressing issues that may arise with jaw movement and overall jaw health.
What are temporomandibular joint disorders?
Generally, scientists group them into three categories:
Myofascial pain – This is the discomfort or pain in the musculature and soft tissues of the jaw.
Internal derangement of the joint – This can be a condyle injury, a dislocated jaw, or a displaced disc.
Arthritis – This is an inflammatory joint disorder that may afflict the temporomandibular joint.
Symptoms can include jaw pain, difficulty chewing, clicking or popping sounds, limited jaw movement, change in upper and lower teeth alignment, and severe pain.
Any of these may occur together and can occur simultaneously with other health issues that exacerbate the disorders or make TMD worse, or mimic them, so consult with your doctor as well as an oral professional when getting a diagnosis.
Oral surgeons are often involved to diagnose and treat TMJ disorders, and other treatments may be considered if initial management is not effective.
So, what causes TMJ?
In many cases, no one knows what causes TMJ. Other times, it is associated with trauma to the jaw. Pain can occur when a disc erodes or becomes unaligned, after impact to the jaw, or from cartilage damage from arthritis. TMJ disorders most commonly occur in women ages 20 to 40, but they can occur in men or women of any age.
How do you know if you have TMJ disorders or jaw pain?
Common symptoms include:
Stiffness of the jaw
Locking jaw or limited movement
Painful clicking or popping in the joint when opening and closing mouth
Change in teeth alignment
Neck aches
A physical therapist may also be involved in the assessment or management of TMJ disorders.
Because TMJ can be difficult to diagnose, seek professional help. Make sure you give your doctor as much information about your pain as possible. After a physical exam, if necessary, he or she can get X-rays, a CT scan, or an MRI to reveal problems with bones and discs. Transcutaneous electrical nerve stimulation may also be used as part of the evaluation or to help relieve TMJ pain.
What are the Treatments for TMJ?

Treatments for TMJ vary widely based on a number of factors. They often begin with sedatives or pain medication and other self care practices, including icing and eating soft foods. Some nonpharmaceutical therapies include:
Physical therapy—exercises to strengthen jaw, ultrasound, heat and ice; some modalities aim to increase blood flow to the joint
Counseling—understanding factors that can increase pain; stress management is an important component
Oral splints—a soft or firm bite guard over teeth
If these measures are not successful or your condition is severe, you should consult a trusted oral surgeon and consider:
Arthrocentesis—a procedure to irrigate fluid through the joint to remove inflammatory byproducts
Injections—corticosteroid or injecting botulinum toxin type A into the chewing muscles can relieve TMJ pain more effectively than medication
Surgery—correction of structural problems within the joint to relieve TMJ pain and restore function
The oral surgeon at Solace Oral Surgery are experts at diagnosing this painful condition. Contact us today to answer any questions.
Nonsurgical Treatments for TMJ

For many people with TMJ disorders, nonsurgical treatments are the first and often most effective step toward relief. Physical therapy is commonly recommended to improve jaw movement, strengthen jaw muscles, and ease pain. Therapists may use manual therapy, exercises, and modalities like moist heat to increase blood flow and promote healing. Oral splints or mouth guards can help prevent teeth grinding and jaw clenching, which are common contributors to TMJ pain. Relaxation techniques, such as meditation and deep breathing, are also beneficial for managing stress, which can make TMD symptoms worse. Over-the-counter medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), are frequently used to relieve pain and reduce inflammation. In some cases, prescription medications like muscle relaxants may be necessary to address ongoing pain or muscle tension. Simple lifestyle changes, such as eating soft foods, avoiding chewing gum, and taking breaks to rest your jaw, can also help relieve TMD symptoms and promote healing without the need for invasive procedures.
Surgical TMJ Treatments
When nonsurgical treatments do not provide sufficient relief, surgical options may be considered for treating TMJ disorders. Surgical treatments can range from minimally invasive procedures like TMJ arthroscopy, where a small thin tube equipped with a camera is inserted into the joint to diagnose and treat issues, to more extensive open joint surgery. These procedures may be necessary to repair or remove damaged tissue, realign the jaw, or eliminate scar tissue that is causing pain and limiting jaw function. In some cases, surgical treatments may involve the placement of implants or other devices to stabilize the jaw joint and restore normal movement. It is important to consult with an experienced oral and maxillofacial surgeon or maxillofacial surgeon to determine which surgical approach is best suited to your specific condition. Surgical treatments are typically reserved for severe cases or when other methods have not been successful in providing pain relief and restoring jaw function.
Temporomandibular disorders can significantly impact your daily life, causing jaw pain, difficulty with jaw movement, and even chronic pain that affects your overall well-being. Fortunately, a wide range of treatment options are available, from nonsurgical treatments like physical therapy, oral splints, and relaxation techniques to surgical treatments such as TMJ arthroscopy and open joint surgery. If you are experiencing symptoms of temporomandibular disorders, it is essential to consult with a healthcare professional, such as a doctor or dentist, to receive an accurate diagnosis and develop a personalized treatment plan. Regular dental check-ups, good oral hygiene, and avoiding habits that strain the jaw joint can help prevent TMD and maintain jaw health. By taking proactive steps and seeking professional guidance, you can relieve TMD symptoms, ease pain, and improve your quality of life. For more information on treatment options and expert care, visit the Cleveland Clinic website or schedule a consultation with a specialist.