Introduction to the Temporomandibular Joint
The temporomandibular joint (TMJ) is one of the most important and complex joints in your body. Located just in front of each ear, it connects your jawbone to the temporal bones of your skull. This unique joint is responsible for controlling jaw movement, allowing you to talk, chew, and yawn with ease. Unlike most joints, the TMJ can move in several directions—up and down, side to side, and even forward and backward—making it essential for everyday activities. Because of its versatility and constant use, the temporomandibular joint is also susceptible to a range of problems, known as temporomandibular disorders (TMDs). Understanding how this joint works and its connection to the temporal bones can help you appreciate the importance of keeping it healthy and recognizing early signs of trouble.
Causes of temporomandibular disorders

TMJ has various causes such as:
At the end of the day, the reasons why a TMD starts are often unclear and may involve a combination of factors, including genetics, stress, individual pain perception, and variations in TMJ structure.
1.1 Trauma
- Direct injury to the jaw or TMJ area.
- Repetitive microtrauma from habits like teeth grinding or jaw clenching.
- Variations in TMJ structure can also contribute to the development of TMJ problems.
1.2 Disease
- Osteoarthritis
- Rheumatoid arthritis
- Ankylosing spondylitis
- Other autoimmune diseases
- Connective tissue disorders
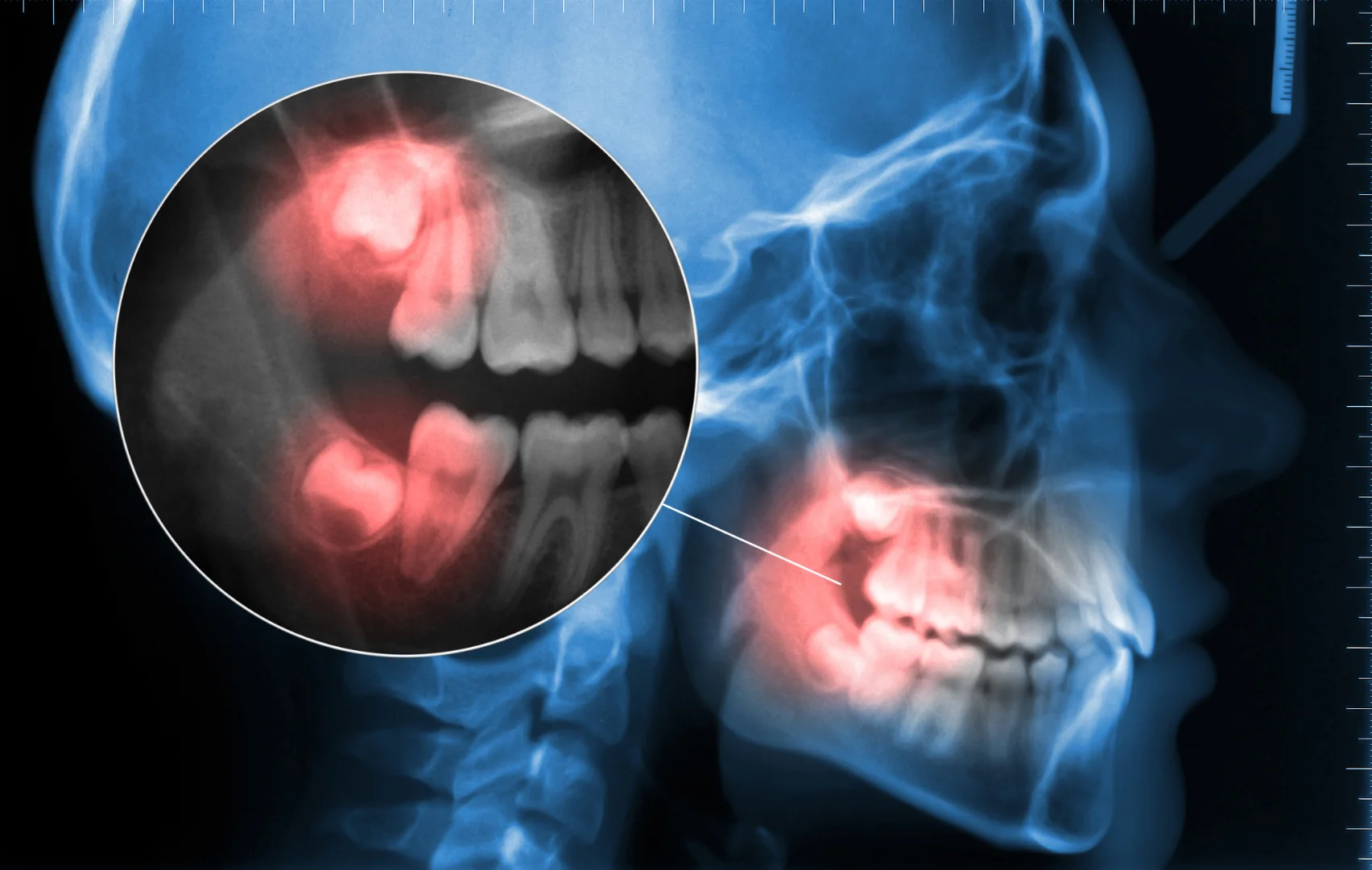
1.3 Dental factors
- Malocclusion (misalignment of teeth)
- Missing teeth
- Poorly fitting dental restorations
Injury
- A hard blow to the face or whiplash
- Pressure on the jaw from clenching or grinding teeth
- Stress that causes facial tightening
Disease
- Arthritis in the jaw (including rheumatoid arthritis and ankylosing spondylitis)
- Sinus infections
- Tooth decay
- Periodontal disease
Symptoms

TMJ symptoms can be painful and may occur on one or both sides of your face. Common symptoms include jaw pain, facial pain, headaches, neck aches, difficulty chewing, clicking or popping sounds in the jaw, and jaw locking, where the jaw becomes stuck or cannot open or close fully. The pain can be temporary or last for years. TMJ affects more women than men and often develops in people between 20 and 40 years old.
Individuals experiencing severe symptoms may require more advanced treatments and should seek specialized care.
Symptoms include: jaw pain
- Discomfort in the face, jaw, neck, shoulders, or ears (when speaking, chewing, or opening mouth)
- Difficulty opening your mouth wide
- Jaw locking (when the jaw becomes stuck or unable to open or close fully)
- Jaw becoming locked in the open or closed position
- Jaw making a popping, clicking, or grating sound when opening or closing mouth (May or may not be associated with pain)
- Face feeling tired or achy
- Neck aches
- Feeling that teeth don’t fit together properly
- Facial swelling
- Toothache
- Headache
- Dizziness
- Earaches
- Ringing in the ears
TMJ Treatment

If your TMJ is not severe, your doctor may suggest:
- Over the counter medications, like ibuprofen or naproxen, to relieve swelling and pain.
- Eat soft foods like soup, eggs, fish, yogurt, and cooked vegetables to reduce strain on the jaw joints. Avoid hard or chewy foods that can worsen TMJ pain.
- Apply an ice pack or use warm, moist compresses to help with swelling and soreness.
- Limiting excessive jaw movement – yawning, yelling, singing, gum chewing
- Keeping upper and lower teeth slightly apart to relieve pressure on the jaw joint and avoid clenching
Physical therapy may include manual therapy techniques that target the soft tissues around the jaw joints to improve mobility and pain relief.
If your case is severe, your doctor may suggest the following treatments:
- Transcutaneous electrical nerve stimulation (TENS) – relaxation therapy of the facial muscles with low-level electrical currents.
- Ultrasound – heat therapy to improve mobility and reduce soreness.
- Injecting botulinum toxin type A into the chewing muscles to help relieve muscle spasms and improve TMD pain, though effectiveness may vary.
- Behavioral health approaches, such as cognitive behavioral therapy and biofeedback, can help identify negative thoughts and physical habits that contribute to TMJ disorders and pain conditions.
- If conservative measures do not provide pain relief, other treatments may be considered, including consultation with oral surgeons for advanced procedures.
- Surgery – as a last option, including implant surgery for severe jaw joint damage (Seek a second or third dentist’s opinion before going this route.
Bite correction may involve adjusting the alignment of upper and lower teeth to improve jaw joint function and reduce TMJ pain.
TMJ disorders can be complex and may coexist with other pain conditions. Treatment goals focus on pain relief and improving TMD pain by addressing issues with the temporomandibular joints, jaw joint, and surrounding structures.
For more help with TMJ or jaw pain, schedule a consultation with Solace implant center & oral surgery.
Managing TMDs with a Healthcare Provider
Working with a healthcare provider is key to effectively managing temporomandibular disorders. The process often begins with a detailed medical history and a thorough examination to pinpoint the underlying causes of your symptoms. Your provider may suggest self-care strategies like eating soft foods, avoiding extreme jaw movements, and applying moist heat or cold packs to ease pain. In addition, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or prescription medications may be used to treat pain and reduce inflammation. For persistent or severe cases, advanced treatments like transcutaneous electrical nerve stimulation (TENS), TMJ arthroscopy, or even open joint surgery might be considered. By working closely with your healthcare provider, you can develop a personalized treatment plan that addresses your specific needs and helps restore normal jaw movements and comfort.